A user research report report on opportunities for tech-enabled innovation in student mental health from Shift and X.
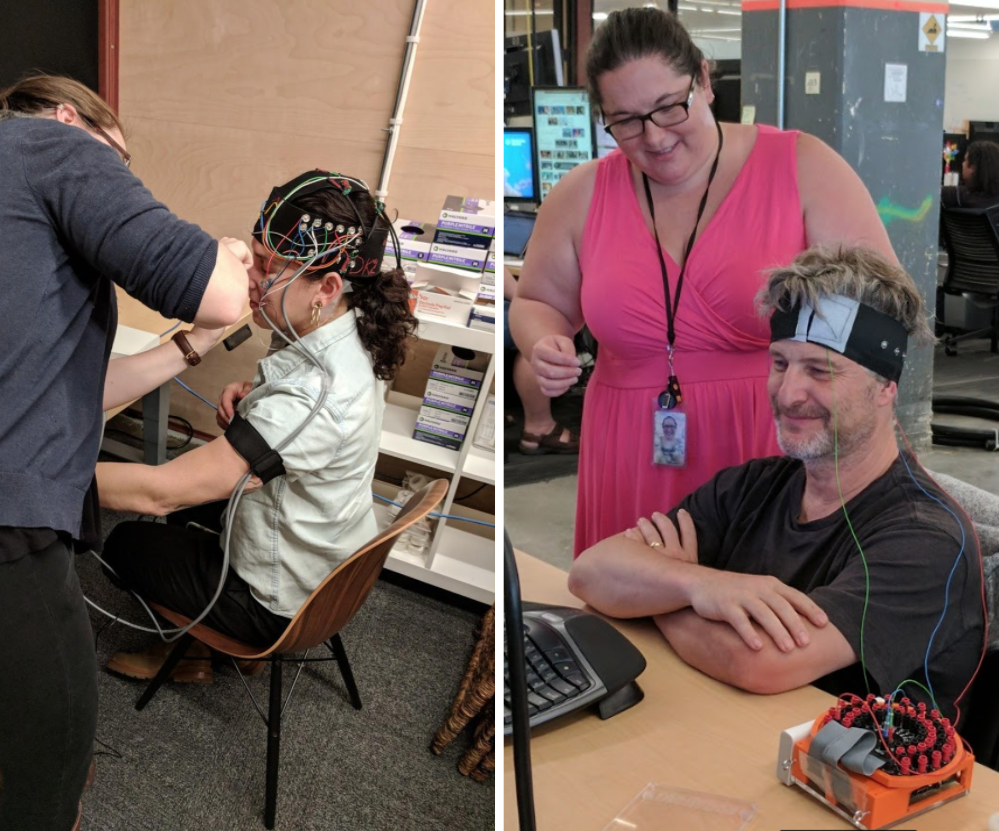
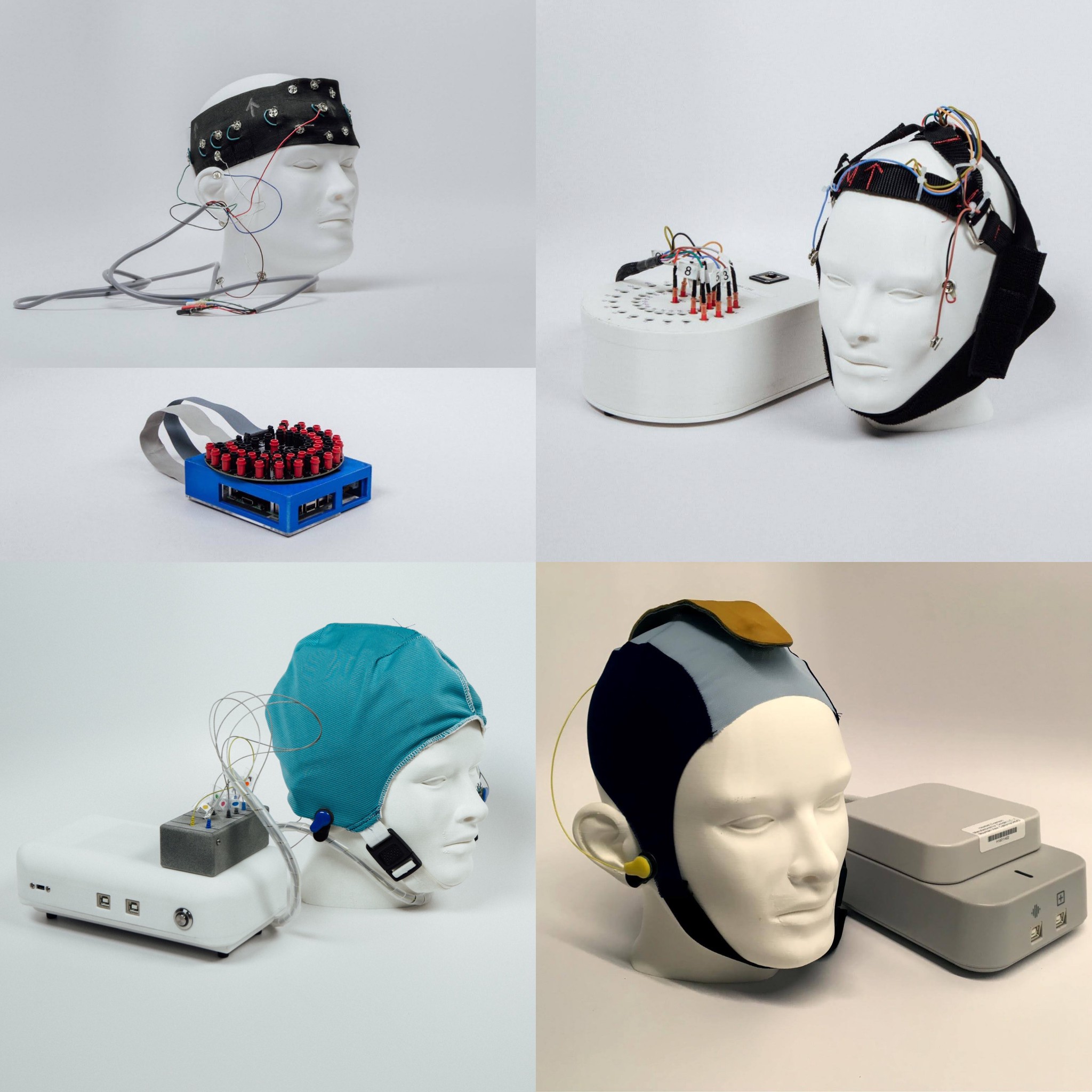
Recently I wrote about Amber, the early stage mental health project I led at X. We developed prototype technologies to better measure mental health, including a low-cost, portable, research-grade system to make it easier to collect electroencephalography (EEG) data, and machine learning methods to make it easier to interpret these data. We wrapped up our work at X and made our technology and insights freely available to the mental health community. You can read more about Amber’s story and access our technical resources on the X blog.
Today we are sharing a report on the user research with students and clinicians that we conducted between 2018 and 2020 in partnership with Shift, a social innovation charity.
Project Amber asked the question: what if we could make brain waves as easy to measure and interpret as blood glucose, and use the results as an objective measurement of depression? From my undergraduate degree in psychology I was familiar with EEG, a 96-year-old technology to measure electrical activity in the brain. Today EEG is primarily used in neuroscience research labs and epilepsy clinics. Making EEG more accessible and usable at scale would open up a host of possibilities to deploy it in primary care, counselling and psychiatry. We had a promising technology, but we had to identify specific user needs to figure out how the technology could impact real-world problems.
We started with informal user interviews, with clinicians and people with lived experience of mental health problems. We spoke with primary care physicians, therapists, counsellors, clinical psychologists, psychiatrists, and social workers. We spent time with young people and their parents, mothers who experienced perinatal depression, and people who had struggled with depression all their life.
In one of my interviews with a physician working in a primary care practice at a London university, I first learned about the huge unmet need in student mental health.
Me: “What percentage of your patient visits are about mental health?”
Dr M: “Seventy percent.”
Me: “Did you say seventeen?”
Dr M: “No, seventy. Most of my patients are students between 18 and 24 years old. They don’t have many health issues other than sexually transmitted diseases and mental health. Around exam times when they get stressed, nearly 100% of my visits are about mental health.”
She told me about her challenges in triaging students in a 10-minute appointment: deciding who will likely get better by themselves, who can be treated within primary care, who to refer to a mental health specialist, or who needs a safety plan because they face immediate risk of harming themselves. 78% of students on her campus self-identified as having some mental health issues. The average waitlist for therapy was 3 months. Every year there were student suicides at her university.
Back at my desk I researched statistics and literature on student mental health, which concurred with Dr M’s experience. There is a crisis on both sides of the Atlantic. Ever greater numbers of students in the UK and US are presenting with mental health problems. Higher education institutions are struggling to keep up with the demand for support. These challenges are exacerbated by a backdrop of multiple societal crises, including the climate emergency, racial injustice, systemic inequity, and now a global pandemic. This means there is great need for change and even greater potential for innovation.
After Kit Yee Au-Yeung joined my team as a product manager, we partnered with Shift, a London-based social innovation charity with experience of user-led design and deep knowledge of the youth mental health space. We commissioned Shift to conduct more formal user research into student mental health to learn more about the experiences of students and clinicians working in higher education settings. In a series of studies between 2018 and 2020, Shift tested how Amber’s proposition of introducing a new, more objective measure of depression and anxiety would resonate with clinicians and students with lived experience of mental health problems: how they might use it in their daily lives and professional practice, and what the challenges might be in introducing such a radical new approach.
We found student mental health to be a fertile ground for tech-enabled innovation for several reasons. There is growing unmet need for college mental health services. Students have been pushing for change in mental health and are often early adopters of technology. Universities have both a moral and financial incentive to improve their student mental health systems.
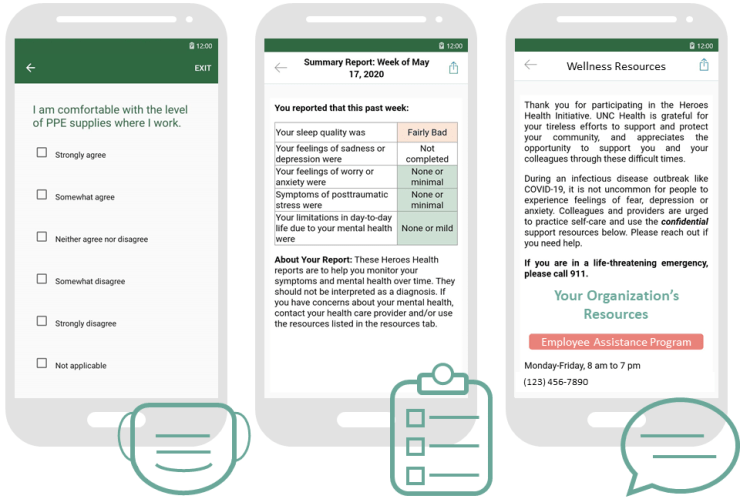
Shift’s report highlights the current challenges in college mental health, the role that better mental health data can play in empowering both students and clinicians, and the importance of putting people at the heart of tech innovation. We emerged with three clear recommendations for those working to improve student mental health:
- Support students to track their own subjective data
- Introduce objective data into therapeutic interactions
- Make data accessible and interpretable for students and clinicians
By sharing our insights as well as open-sourcing our technology, we hope to inform and enhance the work of other researchers and innovators striving to improve mental health services and outcomes for students. We also hope to encourage much-needed investment into further research, tools, and services to improve student mental health, accelerating systemic change towards a world where all students can get the mental health support they need.
Learn more about our user research and download the report on the Shift website.